Fibroids are almost always benign tumors that grow anywhere in the uterus. They occur in at least 25-30% of women of childbearing age and are directly related to the presence of estrogens.
WHEN AND HOW OFTEN THEY APPEAR
There are indications that their appearance is related to a family predisposition, and they occur more frequently in the black race than in the white. The way they are created is not clear, but it does appear that there is a genetic modification in some cells of the uterus that will always, with the presence of estrogen, lead to the appearance of the fibroid. They usually occur for the first time in women 30-40 years of age, but they are unlikely to occur earlier. They almost always shrink with the onset of menopause due to the absence of estrogen and are therefore unlikely to occur for the first time after the age of 50.
THE PLACES THEY APPEAR
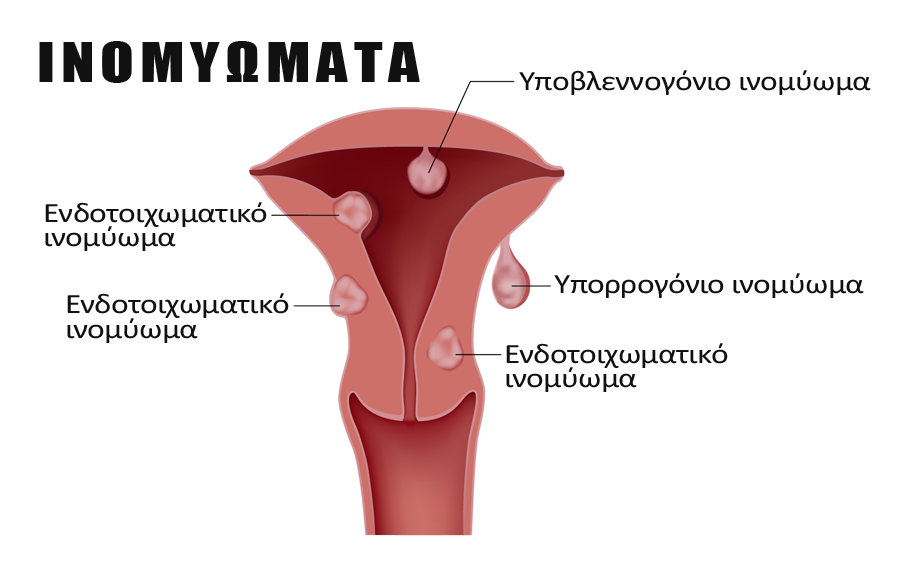
The fibroids can appear anywhere in the uterus and, depending on their location and size, cause different symptoms. They may be:
- Inside the cavity of the uterus they are called submucous. These are the fibroids that cause the most problems because they disturb the endometrium, even if they are small in size, for example 1-2 cm. They can therefore cause menstrual bleeding, difficulty conceiving due to an embryo’s inability to implant, and abortion in the 1st trimester. They should be removed almost always, especially in women of childbearing age. They should be removed hysteroscopically.
- Inside the uterine wall and are called intra-wall. These fibroids rarely cause symptoms unless they grow more than 4-5 cm in length and begin to disrupt the uterine architecture.
- On the outside of the uterus, that is, in the abdomen and are called subserosal fibroids. And these are asymptomatic, unless they grow too large and push adjacent organs into the abdomen, such as the bladder or intestine.
- Rarely they can be found in the cervix or in the wide uterine ligament.
SYMPTOMS AND MONITORING
Most fibroids do not cause any symptoms and are a random finding on a routine ultrasound scan. Because they tend to grow, it is advisable that they are monitored by ultrasound examination every year. If they cause any symptoms, these are period disorders or adjacent organ pressure.
TREATMENT
Treatment is always surgical. Medication has been tried extensively in the past and results in a transient contraction of the fibroids, but they almost always return to their original size upon discontinuation of treatment. Depending on their position in the uterus, the removal can be done hysteroscopically, that is, vaginally using a hysteroscope or laparoscopically. The development of these two techniques has now rarely made the need for open surgery and only in very specific cases. It should be noted that most fibroids do not need to be removed. As long as they do not cause symptoms and do not increase in size, the annual regular checkup is sufficient. In addition, fibroids are benign tumors of the uterus and the chance of becoming malignant is less than one in a thousand cases.
In summary, fibroids should be surgically removed (laparoscopically or hysteroscopically) when:
- They disrupt the inside of the uterine cavity.
- They cause symptoms, such as bleeding, pressure on other organs.
- They are over 4-5 cm, especially in women of childbearing age.
- They significantly increase in size over a short period of time, especially after menopause.
POLYCYSTIC OVARIAN SYNDROME
Polycystic ovarian syndrome is a common hormonal problem in women of childbearing age.
It can occur from adolescence, with lifelong ups and downs and a complex manifestation of symptomology that varies from person to person. The name denotes “many cysts in the ovaries”, but it’s certainly much more than that. In this sense, the term is often misused, and caution is needed here.
Key elements of the syndrome are:
-Disturbance of the cycle in the form of araiominorroia (there is a systematic delay in menstruation, from days to months). This is due to anovulatory cycles and leads to
– Infertility
– Acne and hair loss
-Increase of body weight or inability to lose it
The (usually young) woman comes to the gynecologist reporting some or all of the above mentioned problems. Detailed history, clinical examination, ultrasound and blood tests are required to make the initial diagnosis, assess the severity, and then periodically examine the patient’s progress.
Increased androgens (testosterone) and FSH / LH ratio disturbance (these are produced in the brain and are related to ovarian function and ovulation) are classic findings. Thyroid and prolactin control are essential. Central to the mechanism of the disorder is the cell’s resistance to insulin (a hormone that regulates glucose consumption by the cell). This leads to hyperinsulinemia and predisposition to diabetes mellitus. A glucose curve and referral should be made if necessary, to a nutritionist and endocrinologist.
Treatment
Polycystic ovarian syndrome is a functional disorder with a variety of symptoms that negatively affect the emotional state. Stress in turn exacerbates the symptoms of the syndrome. The therapeutic approach must consider the above and suggest ways of managing stress.
It is emphasized that lifestyle change, with good nutrition and exercise leading to weight loss is particularly important, because in addition to its direct effect on the mechanism of POS, it will indirectly improve the emotional state of the woman.
Common interventions include:
-As mentioned earlier, the cornerstone of treatment is weight loss and physical activity, which will stimulate the metabolism and improve the woman’s hormonal profile. The adipose tissue is involved in the regulation of androgens and insulin-glucose.
–Use of contraceptives: the cycle will be restored immediately. It is advisable to recommend thrombophilia screening. It takes at least one semester for acne and hair loss to be visible, so the patient must be patient. Here the combination of contraceptives with antiandrogens can provide additional help. Gradually there will be a remission of symptoms and this will work encouragingly. Dermatologist solutions (hair removal, laser) can be used in the meantime.
-If there are contraindications to contraception, a long delay (even after pregnancy is excluded) may result in a period of few days of taking progesterone pills. This will prevent endometrial hyperplasia and abnormal bleeding.
–Metformin (glucophage).
–Dietary supplements (inositol) that act at the cellular level, reduce insulin resistance and lead to a decrease in androgens.
-In terms of infertility, the goal is to restore ovulation. If physical conception is not achieved despite weight loss, cycle adjustment and remission of other symptoms, then treatment with clomiphene pills or injectable formulations aims to induce ovulation. Here you will need close control because women with polycystic ovaries tend to have ovarian hyperstimulation.