The stages of In Vitro Fertilization, from the first visit to the specialist until conception.
Consulting visit to the specialist
To be able to talk about infertility, a couple must not have conceived after a year of free sexual intercourse. This period is limited to six months if the woman is older than 37 years.
At the first visit to the doctor’s office, it is a good idea for both members of the couple to come, having the comfort of time and presenting possible examinations that have been performed so far. The doctor will take a detailed history from both of them. A gynecological examination and transvaginal ultrasound will follow, while if the male factor is probable as a cause of infertility, an examination of the man can also be performed.
If the couple or the woman is away – or due to special circumstances that do not allow a visit to the doctor’s office – the first meeting with the doctor can be made by teleconference and can be just as effective. In this case, the doctor will see the tests that have already been performed and may request additional tests that can be done at the couple’s place of residence.
Examinations to determine the causes of infertility
Depending on the findings of the first examination, hormonal blood tests are prescribed for the woman on the second or third day of the period and vaginal ultrasound on the third day of the cycle.
In most cases it is necessary to perform hysterosalpingography, i.e. an x-ray with which the anatomy of the uterine cavity and the patency of the fallopian tubes are checked.
The history and findings of the above examinations will determine whether more specialized examinations will be performed, such as karyotype, thrombophilia screen, hysteroscopy or laparoscopy.
Tests for men include a sperm test, that is, a sperm chart, a sperm activation test, and a sperm culture. An ultrasound of the scrotum may also be performed.
All examinations can be performed either in the IVF unit or in any other diagnostic center, while in most cases they can be performed in the couple’s place of residence.
After the examinations, their results are evaluated and in collaboration with the couple the doctor determines an action plan. This plan may include alternative therapies or lead directly to in vitro fertilization.
Initiation of IVF – Ovarian stimulation
The first stage of IVF is the controlled stimulation of the ovaries in order to produce more than one follicle – eggs. This is done through the administration of hormone drugs, which encourage the completion of the development of the original follicles. It is important to emphasize that ovarian stimulation does not lead to premature menopause even if repeated several times. The reason is that the eggs produced would be destroyed anyway during this cycle.
Oocyte Maturation
The maturation of the follicles is monitored with frequent ultrasounds and measurements made on specific hormones in the blood. The goal is their optimal growth that lasts about 9 to 12 days. After this period, a final injection is given for the final oocyte maturation, followed by ovulation after 34 to 36 hours.
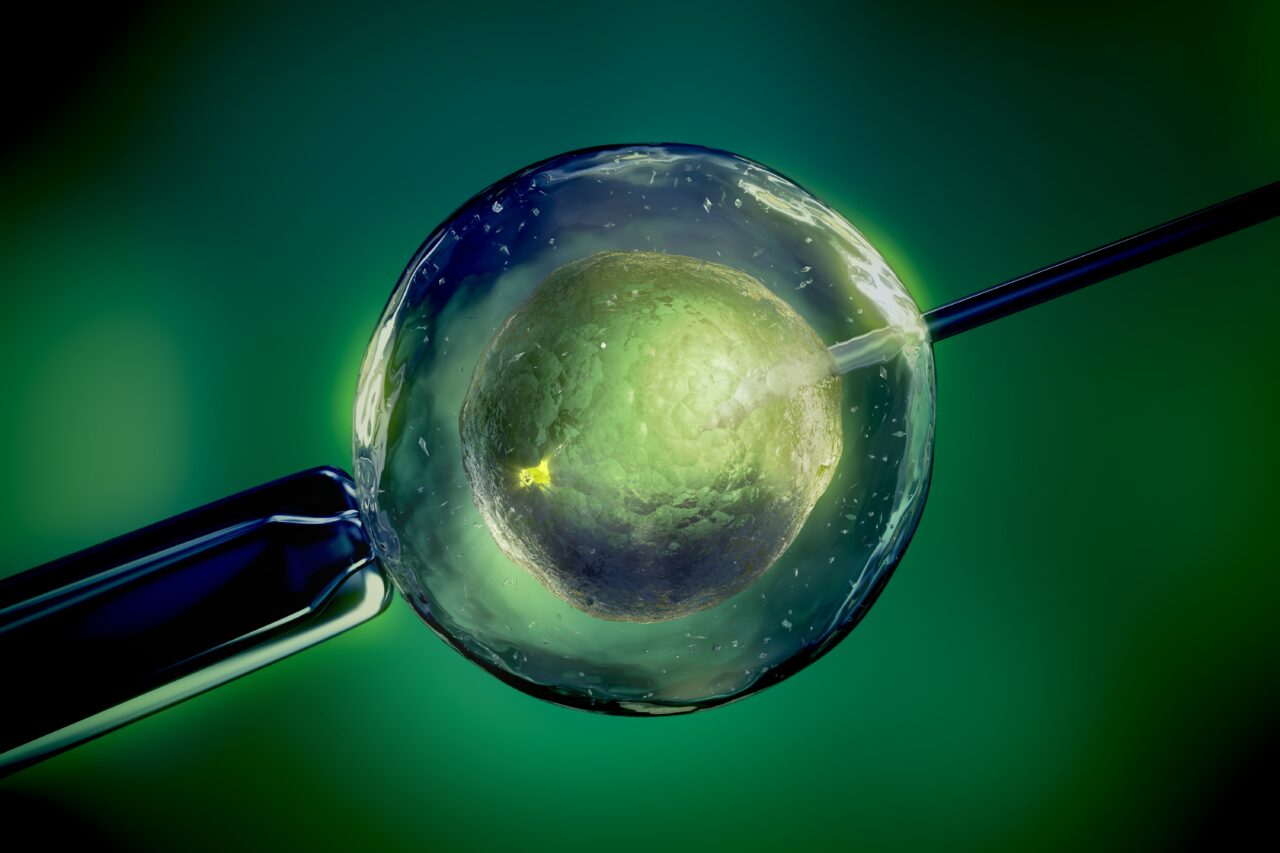
Egg Retrieval Process and Sperm Collection
Retrieving the eggs from the ovaries takes about 30 minutes and is done using intravenous analgesia – intoxication so that it is practically painless. The doctor has a continuous image of the ovaries through transvaginal ultrasound and inserts a thin needle that penetrates the vaginal wall and punctures the follicles. The contents of each follicle are delivered to the embryological laboratory, where the embryologist examines the follicular fluid under a microscope, locates and collects the eggs. After the egg retrieval the woman remains in the unit for 1 to 2 hours and then she is able to leave.
The woman’s partner delivers a sperm sample to the lab on the same day of egg retrieval. The best collection method is masturbation and the procedure takes place in a specially designed space in the IVF unit, with all the conditions of hygiene and discretion. It is important to have two to five days of abstinence from any sexual intercourse. The sperm sample is processed and the most mobile and morphologically normal sperm are collected in a small volume of culture material.
In vitro fertilization (IVF)
If conventional in vitro fertilization (IVF) is selected rather than micro-fertilization (ICSI), the eggs are fertilized by placing them together with a certain number of activated sperm of the partner in plates with special cultivation material and incubated under strictly controlled cultivation conditions. Essentially, the sperm are left to fertilize the egg on their own, without any intervention on the part of the embryologist.
Embryo transfer
Before embryo transfer, embryologists examine the embryos, which may be fresh or thawed, for abnormalities in the number or structure of their chromosomes (e.g. Down syndrome) and for specific genetic conditions, such as Mediterranean anemia, cystic fibrosis and muscular dystrophy. In addition, in very specific cases – and before the embryo is frozen, if this choice is made – a preimplantation genetic diagnosis can be made.
During embryo transfer, two to three days after egg retrieval or five to six days after egg retrieval once the embryos have reached the blastocyst stage, the embryos are transferred and deposited in the uterine cavity.
Their selection is made by the embryologist in collaboration with the doctor. The best ones are selected based on their morphology and the embryo transfer of one or two embryos takes place. The doctor decides either to proceed with the embryo transfer of fresh embryos, by freezing the rest or to freeze all the embryos (freeze all) and the embryo transfer to be done next month.
The embryo transfer is performed as follows: the embryologist aspirates the embryos in a special catheter and the gynecologist, with the help of abdominal ultrasound, inserts the catheter into the uterine cavity where they leave the embryos with extremely gentle movements. The procedure is painless, takes about 15 minutes and does not require anesthesia. The woman remains lying in the unit for about 1 hour.
Ten days after embryo transfer, if 5th day embryos (or blastocysts) are selected, or 12 days if 3rd day embryos are selected, blood hormone β-Chorionic Gonadotropin (β-CG) is measured to determine whether or not pregnancy has been achieved.
Embryo Cryopreservation
Excess, good quality embryos that are not transferred to the woman’s uterus can be frozen to ensure a second embryo transfer, in case the first one does not succeed. Cryopreservation also offers the opportunity to have a second child without having to re-stimulate the ovaries or retrieve other eggs.